Socio-technical approach to community health: designing and developing a mobile care data application for home-based healthcare, in South Africa
1. Introduction
The aim of this report is to describe the design and development considerations related to a mobile home-based healthcare application for care givers in a community in the Western Cape, South Africa. In order to do this we first describe current practices of health care givers in the Western Cape in capturing and reporting the data of their patients in practice. Although the overall aims of home-based healthcare are the same everywhere in the world, the context of a particular country is important because it determines how home-based healthcare is implemented in practice. In this instance the design and development of the mobile care data application were undertaken by a local university as part of a funded project to stimulate innovation by using informatics to address real needs in communities.
The main question focused on in this report is: From a socio-technical perspective, what are the considerations for designing and developing a mobile application to facilitate the capturing and processing of patient data by care givers in a particular community? The supporting sub questions are: What are the contextual aspects that need to be considered for the introduction of m-health solutions? How did the university doing the development work engage with communities to ensure sufficient participation in specific projects? How did care givers participate in the design and development process of mobile solutions? How the mobile user interface was designed according to the care givers' preferences of using mobile phones? The study therefore centered on the interaction between the university and the care givers.
For this study service design methods were used to determine the design considerations since these provide a mechanism to depict a service path and ways for understanding the different stakeholder experiences' of the service. Only once it was understood how care givers interact with patient data, was it possible to design the mobile user interface. A socio-technical approach was adopted and the reasons for using this approach are discussed in the Materials and Methods section.
The literature review in the next section provides context on home-based healthcare in general and more specifically in South Africa. This is followed by a section on community engagement in general and how universities should engage with communities around innovation. The literature review is concluded with aspects of mobile health (mHealth) and how patient records have been used to identify all the issues that were important for this study.
The remainder of the report is organized to explain the methods and materials, followed by the results and a discussion of the results. The report is concluded with what the results mean and with suggestions for further research.
2. Related Research
The literature review highlights relevant considerations indicated by other studies for this research study. The main theoretical concepts for this study are the mobile care data application (mHealth), the user of this application (care giver) in the context of home-based healthcare for a specific community and design and development by university students as part of university-community engagement. The sub sections for this section are therefore home-based healthcare, community engagement, mHealth and patient records.
2.1 Home-based Healthcare
Home-Based Healthcare (HBHC) also referred to as Home Based Care (HBC) is the provision of basic nursing care needs by trained or informal semi-trained caregivers to people in their own homes. This service is available to people who have mental, physical, emotional and social needs. HBHC is particularly relevant to Third World countries whose public health systems and facilities cannot keep up with the growing needs of the population (WHO, 2004).
The need for HBHC in South Africa is enormously high due to HIV/Aids, TB, cancer and other chronic illnesses. A large part of the population lives in rural areas cut off from services and infrastructure as well as overburdened public facilities substantiates the reason for HBHC as such an important aspect of primary health care in South Africa. In South Africa these services are provided by local non-profit, non-governmental organizations. The Department of Health of the Government of the Western Cape Province in South Africa indicated their commitment in their annual performance plan 2011/2012 to manage the burden of disease with an improved integrated community health care service delivery to address the Millennium Development Goals 4, 5 and 6.
Tanser et al. (2001) state that good health system management relies on informed decisions regarding resource allocation. Decisions often occur in the absence of data that allow the pattern of resource allocation to be assessed. Data collection and analysis are therefore of great importance to the improvement of health care services at an HBHC level of delivery. However, data recording in HBHC is problematic for many reasons such as caregivers in the communities' use of paper-based data recording, which is both time consuming to record and to process and the paper-based data being prone to getting lost or damaged by environmental factors like rain. Electronic data collection is hampered because access to computers is very limited and computer literacy is scarce. Mobile/Cellular phones are however common, most NGO caregivers are required to own one for communication with supervisors. This opens up opportunities for the use of mobile devices for the collection of data.
2.2 Community Engagement by tertiary institutions
Although admittedly community engagement by health institutions in general is important, the primary engagement relationship that is of importance in this instance is the engagement by a university with the care workers in a community. Therefore this section examines literature that relates to engagement by tertiary institutions.
In poorer communities the position of the individual is never separate from the community to which the person belongs, e.g. care givers operating in groups and visiting patients/clients where often family members, friends or neighbors are present during the visit (van Zyl, 2010). The condition of the individual, health or poverty related, becomes a collective problem where others in the community take up the responsibility of caring for those in need even if these persons themselves experience difficulties - this became evident from the findings of an ethnographic study on home-based healthcare (Van Zyl, 2010). Negative health-related impacts on the community include violence, substance abuse, sexual violence, early onset of sexual activity and teenage pregnancy (Mosavel, et al., 2005).Some positive aspects identified in their study are the joy and pride of individuals who are able to make a difference in others' lives and the strong support networks of friends and family.
A community-based participatory research (CBPR) framework was developed by Mosavel, et al. (2005:2578) to negotiate a mutual agenda between communities and researchers to ensure that the research is relevant to the communities. Their framework incorporates the communities concerns and priorities while stressing the intersecting roles of poverty, violence and other cultural forces that impact the health and wellbeing of the community members. Lavery et al. (2010) suggest that guidelines are required to deal with the role of communities for the evaluation of new technologies in global health for meaningful community engagement.
The success of the proposed collaborative university-community network will depend on the stability of the network and this will be the case if more actors from both the university and community "join" the network because they want to align their interest to that of the network.
2.3 Mobile Health
Mobile Health (mHealth) is a component of eHealth and to date no standardized definition of mHealth has been established. Global Observatory for eHealth (GOe) defines mHealth as "medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices" (WHO, 2011). The core utility of the mobile phone, voice and text messaging, can be used as well as more complex functionalities and applications including general packet radio service (GPRS); third and fourth generation mobile telecommunications (3G and 4G systems); global positioning system (GPS); and Bluetooth technology. In 2011 there were an estimated 5.9 billion mobile subscriptions worldwide (International Telecommunications Union, 2011).
In spite of the many benefits that mHealth could offer in healthcare, most mobile applications are still primarily in developmental and pilot use stages with many issues still not well understood (Maglaveras, et al., 2002; & Rice, 2009; Lee et al., 2009; Svanæs et al., 2008).There are therefore not yet extensively documented best practices that could guide the design and development of mobile applications and there are still many complexities associated with this type of technology that could influence the design, development and eventual adoption of mobile solutions. In spite of this, in the case of South African home-based healthcare situations, mHealth applications are potentially viable because the extremely high penetration rate of mobile phones in the country means that there is the potential for the many care givers who own mobile phones to potentially capture patient data at the point of care.
Since mHealth is a component of eHealth it should not be seen as a possible replacement of eHealth but rather an extension of certain aspects of Health (in the broadest sense), e.g., the mobile interface providing additional possibilities to capture and access data at other locations than where the patient folder is kept (paper-based) or where the workstations are located (eHealth). In practice a mix of different approaches, will probably be used in order to, for example, utilise the 'ecological flexibility' (Berg, 1999) of paper documents in conjunction with electronic and mobile systems.
2.4 Patient Records
Patient records are used in healthcare for coordination and cooperation of a large collection of healthcare stakeholders that form large and complex networks (Berg & Bowker, 1997; Hanseth & Monteiro, 1997; Fitzpatrick, 2000). Healthcare records, or in this case patient records, are configured according to the needs and practices of the organizations they serve. Patient records are used over time by different stakeholders for different purposes and in different ways. The nature of what and how data is captured and used in patient records reflects the highly subjective judgments of their users, e.g., the, care givers, etc. Although there are many initiatives and market trends to convert patient records to electronic records, in reality most healthcare organizations still use a mixture of paper-based and electronic patient records (Saleem, et al., 2009). The focus of this study is not on the merits of paper-based versus electronic patient records but rather on how the patient record is used during interactions of healthcare data stakeholders and patients. Little evidence was found in literature to indicate what constitutes a mobile health record (MHR). The nature of the workflow in providing home-based healthcare services will determine how data is structured and used in any mobile solution.
3. Materials and Methods
3.1 Socio-technical Approaches
Carayon (2006) considers the trends of working across organisational, geographical, cultural and temporal boundaries and the increasing role of the customer (in this case the care giver) in product/service design that contribute to increased work system complexity. Patients, families and care givers are becoming increasingly co-collaborators in home-based healthcare services and this collaboration with healthcare service providers will influence the way technology is incorporated into home-based healthcare service provision. There is a need for developing principles for the design of socio-technical systems in addition to considering the impact of such systems on people (Carayon, 2006). He indicated that further research is required to understand the work of designers of socio-technical systems and to identify or develop methods that can help to improve their design. These methods need to consider how, for example, care givers, could become active collaborators in designing ICT solutions. During the implementation of socio-technical systems the following need to be considered: issues of participation; feedback; training and learning; project management; and organisational support and management commitment (Carayon, 2006).Ghaffarian (2011) argues that new socio-technical approaches in Information Systems (IS) research can capture the contingencies of contexts and situatedness of actions.
3.2 Research Methodology
This is an interpretive study to explore and understand the design and use of home-based health records in a community in South Africa. The research strategy was an ethnographic study and the qualitative methods to collect the data have been observations, in-depth interviews and studying of documents and artifacts. During the observations the emphasis was on how the caregivers and healthcare professionals provide a care service to patients at their homes. A specific consideration was how caregivers use and record data and how healthcare professionals utilize data.
The research design provided for various activities that included pre-work and fieldwork where a team of students, including designers and IT developers were assembled, the study of home-based healthcare literature and documents, discussions with HBHC stakeholders that enhanced the understanding of HBHC, and the selection of a specific community in the Boland (in the vicinity of Cape Town) that was accessible and affected by many of the social-economic factors evident in South Africa (e.g. poverty, crime and disease) was selected.
A further step was to describe and analyze the "home-based care landscape" to depict the organizations, political structures, stakeholders and relationships between them. As part of context mapping, a service design method, the activities and services of HBHC were identified to depict the care path available to the citizens of that community. The purpose of context mapping is to reveal the users' conscious and latent needs, experiences, hope and expectations.
Service design addressed the care service from the clients' perspectives with the aim to ensure that care service interfaces are useful, usable and desirable from the client's point of view and effective, efficient and distinctive from the supplier's point of view (Miettinen, 2009). Although the client in HBHC is primarily the patient, the informal care giver who supports the patient, in most cases family members, friends or neighbors, as well as the caregiver can also be regarded as the client of the service. For the purpose of this study the caregiver is considered as the main client with the patient and supporters the main beneficiaries and the healthcare facility the supplier providing the care service. The healthcare facility for this study is a hospice (which in South Africa refers to a non-governmental body that provides dignified care and support to patients that are either terminally ill or suffer from life-threatening diseases) and the main stakeholders working for the hospice are the healthcare professionals, the sisters, administrative personnel and managers.
Next as part of a service design approach, the method of observation and documentation was used as part of the ethnographic study. The care service of a caregiver to two patients at their homes was filmed. The camera "followed" the care giver and recorded the care process. This allowed the researchers to study the process in more detail to also uncover the activities that happened in the background. Other service design methods used was scenario-based design to develop specific scenarios and touch-points for HBHC - this was done by developing storyboards with the users, context and a story with a specific background, tasks, goals and actions. A low-fi prototype was used to determine the flow and navigation of the data for the mobile interface. With this method the caregivers became co-designers of the mobile interface. The results presented by these different design methods were analyzed to identify problems experienced by the caregiver when interacting with the patient record or care reports.
The interns used an agile approach to develop the mobile interface and they were interviewed to determine their experiences during the development process. They were able to indicate the problems experienced during the process as well how they interacted with others. The testing of mobile interface and back-end systems were investigated through observations and interviews.
The results were analyzed and interpreted to derive the findings and obtain deeper insights of how the design and development of the mobile interface happened in practice.
4. Results
4.1 Data and service flows
The township community suffers from the socio-economic factors that influence the wellbeing of a community. There is a high incidence of HIV/AIDS and TB and the home-based care needs are typical of a poor community. The caregivers are citizens from the township who have received basic home-based care training. The hospice is responsible for the home-based care service to ten areas representing communities in a town in the Boland in the Western Cape, South Africa and its immediate surroundings. The township selected for the ethnographic study is one of the poorer areas. Figure 1 is a photo of the "homes" in the township.
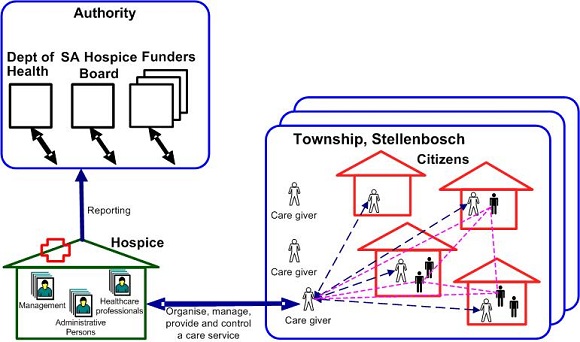
The hospice reports to the Department of Health, the South African hospice board and several funding organisations providing funding for the service. The landscape of the community is illustrated in Figure 2. The organisational structure at the facility is as follows: the patient care manager is responsible for the service to the patients. A senior coordinator is responsible for all the caregivers and they replay all information to her. Each area is coordinated by a caregiver or enrolled nursing aid and they see the caregivers on a daily basis. Each area is serviced by a qualified sister who is responsible for the initial assessment of the patient and continuous progress of the care plan. A copy of the care plan is left at the home of the patient as well as at the facility. Each care plan is revised every three months which means that the care plan is collected from the patient's home and brought to the facility.
The caregiver completes a daily care report after each visit of a client and a copy is usually left with the patient. Once a month the care giver is required to summarize the daily care data on a monthly care report. This is problematic and time consuming since many of the caregivers have limited literacy skills and find it difficult to transfer and calculate the data from one form to the next. Headings often appear in columns in one form and then in rows for the next.
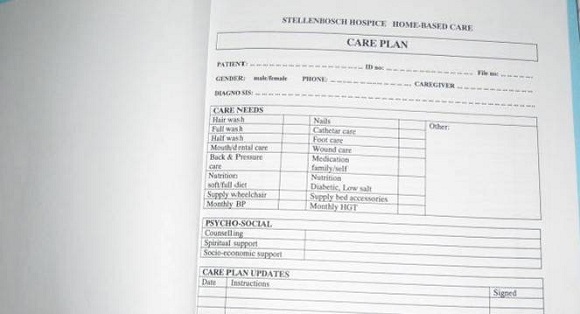
Figure 3 shows a care plan that needs to be followed by the caregiver for the specific patient. Much of this is duplicated daily as the caregiver visits patients just to demonstrate adherence to the plan with patient signatures required as proof.
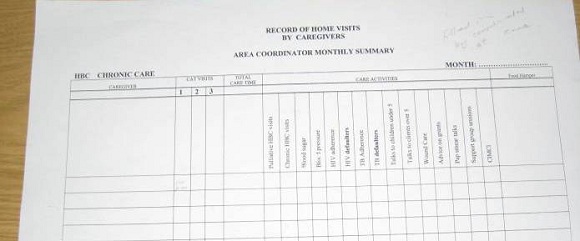
The healthcare professional in this community mainly deals with the patient's care data, i.e. the initial and ongoing assessments based on the patient's condition. The caregiver carries out the care plan which guides the caregiver in what type of care the patient requires. Caregivers capture during their visits their observations and submit a daily report to the facility. The patient may want more information about his/her condition and progress whilst the primary caregiver supporting the patient may need more information about the patient's condition and care requirements and may also want to share experiences with other primary caregivers. The caregiver supervisor collects the forms with the data from all the caregivers and processes these to prepare the patient and visit summary reports.
4.2 Issues and problems experienced by caregivers
The following were found during the investigation: In the home-based care service path little to no attention is given to the caregiver's data recording and communication needs; patients and their supporters have little to no access to useful information that may be relevant to their care; data recording and processing is still manual resulting in many hours spent by caregivers and administrators on these activities rather than the care service; reporting of cases is cumbersome because access to data is not easy and processing is still mostly manual; managers do not have sufficient quality data to manage their caregivers' visits.
It is clear that the current manual data capturing process with paper forms and reports does not support the needs of a sufficient care service and in fact is complicating the care process.
4.3 Development of prototype through co-design
A lo-fi prototype, with a cardboard template of a mobile phone was used. Caregivers enjoyed this method that allowed them to provide input and give their preferences without them being confronted by technology. Figure 5 illustrates this method.
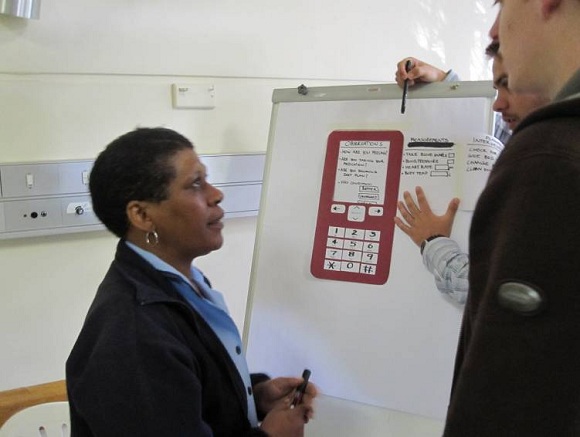
The findings from this co-design activity are: Initially the caregivers were skeptic of the phone capability; lo-fidelity prototypes are easy to understand; it helped to understand their navigation and data entering preferences - they preferred not to enter text but use drop down lists and selection boxes; they were excited about the digital memory and automatic functional advantages. Findings specific to the method are that hand drawn materials are friendlier than hard coded technology, hand drawn materials are more susceptible to change than hard coded technology, and paper prototyping saves valuable time on programming.
Once the data elements to be captured were identified and the navigation of the sequence of capturing the data elements was sufficiently understood the developers continued with the implementation of the prototype of the mobile interface.
The development of the mobile application was done with JAVA, combined with an open source Database Management System.
The developers found their active involvement during the design with the caregivers extremely useful. The initial prototype with the mobile phone and hard-coded interface was sufficient to get an idea of how the interface would work but could not support the additional functionality required for the mobile interface to work in practice. A complete redesign of the back-end to the mobile solution was needed and this was difficult because of all the constraints of the mobile interface. Many problems were experienced, e.g., programming for the different handsets used by the care givers that were not smart phones but feature phones with limited functionality; and the impact of network availability and cost of data transmission on decisions for transmitting data.
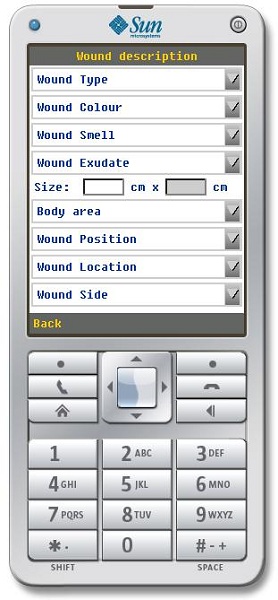
The findings of the development phase are: (1) the role of designer was crucial to obtain a good understanding of how to design an appropriate mobile interface; (2) the translation of the mobile interface design to code was difficult because the limitations of mobile phones used as well as the level of the users presented serious constraints on what was possible and appropriate; (3) different versions of code is necessary to support the different mobile phones used; (4) network coverage and availability is an important consideration that influences how and when data is transmitted; (5) the translation from the emulators used to develop the mobile application on a personal computer to the actual phone did not always produce the same results on the mobile phone; (6) it was difficult for team members to understand what each other has done and to learn how to use the new development tools; and (7) testing was much more difficult than expected where mobile applications introduce more variables to consider during testing.
The team of interns working on this project represented different disciplines (information technology, design and social sciences), different levels (third year, BTech and masters students; different nationalities and cultures (Xhosa, English, Afrikaans, Lusophone (Portuguese), Francophone (Cameroon, Democratic Republic of Congo), Anglophone (South Africa, Nigeria). The diversity of the team contributed significantly towards a better understanding of and sensitivity for context and the role of humans and environment in the design and development of technology solutions. The findings specific to the team are: (1) the inclusion of non-IT persons in IT development adds much value with a better understanding of the problem setting and the persons who will use the solutions resulting in more appropriate and relevant solutions; (2) the diversity of the team resulted in a better understanding of each other's role in the team and exposed them to many alternative views; (3) mentoring of more junior members by the more senior students happened automatically; and (4) all the students indicated that their involvement in the project exposing them to the difficulties experienced in communities in stress allowed them to become better people with more appreciation of their role in technology development.
5. Discussion
The current paper health record, forms and reports do not support an effective home-based healthcare service. Digitalizing the reporting part will certainly allow more time for patient care. A service design approach considers the entire user experience. In the case of home-based healthcare the following user experiences were considered: the caregiver (main focus of the project), but also in at a secondary level (in this instance) the experiences of the patient, the patient's supporter and the healthcare professional. By considering all the service moments and touch-points it is possible to identify the areas that need to be improved. Capturing data is then only one part of the user experience but is influenced by the other parts. The design for a data recording device therefore needs to become part of the user experience by improving the experience. This is only possible if the needs of the user, in this case the caregiver, are sufficiently understood. This confirms the importance of considering situatedness of the care givers during their work practices to obtain a better idea of designing appropriate user interfaces for that specific context.
The different interfaces to support the different care activities support the notion that a health record can never just be a single entity. It is a collection of different components used by different persons for different purposes. It would therefore make sense to rather identify all the possible data elements that can possibly be part of a health record and then only map those that are relevant for a particular service moment to the interface that supports that interaction moment.
The design considerations are summarized as: (1) the home-based healthcare record should be designed in such a way that it supports the different user experiences; (2) useful interfaces need to be designed to ensure better adoption by the user; (3) only the data elements required for that service moment should be mapped to the interface; (4) it is important to understand who the user is before designing interfaces, records, reports, etc. that they will use; (5) it is important to consider other communication modes than text, e.g., visual communication, to cater for illiterate users; (6) the context of the community is very important because the social complexities will determine how the solution should be designed; (7) the design should consider cost restrictions and the need for only basic functionality; the design should support the entire care service path where all the service moments provide for different activities and use of devices/technologies. These considerations should guide the development of the different concepts and prototypes and the user (caregiver, patient, supporter, healthcare professional, authority, etc.) should be actively involved in the process as a co-designer.
By first obtaining a sufficient understanding of the problem setting and the people who will be using the mobile solution a better understanding of the needs can be achieved. During the requirements elicitation process it is important that the users, in this case the care givers, become active co-designers with the designer, who has a good understanding of using the design techniques and with the involvement of the developers. The design of the technology part of the mobile solution is not simple and sufficient attention should be given to this aspect to ensure that all the complexities are sufficiently considered.
Further research is required to investigate how the users interact with the different concepts and prototypes to allow for refinement and fine-tuning of the solutions. The different interfaces will support access to the health record components and further research is also required to determine how the methods used to design and develop a mobile solution for a specific group within a specific community can be used for adapting to other contexts. Security and privacy implications for mobile home-based healthcare solutions also need to be considered in addition to interoperability and standards.
The active involvement of the care givers strengthen the relationship between the community and university and by recognizing the community members' input contributed towards a sense of empowerment. The university interns gained from their involvement in this project by learning from each other and learning to value the users' input. It is therefore possible to have a meaningful university-community engagement as involved partners in designing useful innovative ICT solutions.
6. Conclusion
Through observation, user profiling and participation of the users, understanding of the service design challenges experienced by care workers in HBHC can be constructed. Iterative propositioning, prototyping and experiment are methods used to describe and create patterns underlying the user behavior (Miettinen & Koivisto 2009). Patient records used by HBHC and the data collection for the purpose of these records need to be critically analysed. The use of innovative sociotechnical methods has the potential of realising restructuring and design solutions. Technologies used to achieve this should be appropriate to the context of its intended use. Supportive networks and sustainable systems are required if they are to be useful in the long-term. Further research in this direction holds significant potential for useful outcomes.